Nasal Decolonisation Of Mrsa : Nasal decolonization: What antimicrobials are most effective
Di: Jacob
Oral antibiotic options for treating skin and soft-tissue infections in patients with community-associated MRSA include clindamycin, trimethoprim/sulfamethoxazole (TMP/SMX; . Abnormal skin or wound Small superficial lesions may be treated with mupirocin 2% cream used eight hourly. Staphylococcus aureus in the nose is a risk factor for endogenous staphylococcal infection. Intranasal mupirocin is effective pre-operatively for . Eliminate nasal carriage by prescribing Naseptin ® cream (chlorhexidine plus neomycin), four times a day for 10 days.Schlagwörter:Nasal DecolonizationDecolonization ProtocolMrsa Decolonization 1 Since 1930, the epidemiology of S aureus has changed dramatically, and methicillin-resistant S aureus (MRSA) has reached epidemic levels in both hospitals and community settings.Nasal and skin decolonisation.Schlagwörter:Staphylococcus Aureus DecolonizationNasal Decolonization Prior To Surgery
Nasal Decolonisation of MRSA
Whilst routine universal screening of all potential inpatients is .There is strong evidence that nasal and skin decolonization prior to cardiac and orthopedic surgery is effective in reducing SSIs caused by MSSA or MRSA. Hence, the objective of this meta-analysis . Screening patients for S aureus nasal carriage and . These germs can live on your skin and in your nose.Decolonization Methods (MRSA and MSSA) Short-term nasal application of mupirocin prior to joint replacement surgery (3 times a day for 5 days). 2–6 With the changing epidemiology of MRSA, .Nasal povidone-iodine, alcohol-based nasal antiseptic, and photodynamic therapy are promising new interventions, but more studies are needed.
ERADICATION OF MRSA COLONISATION
Targeted nasal decolonization with mupirocin combined with chlorhexidine body wash may also reduce S.There is strong evidence that nasal and skin decolonization (nasal mupirocin plus CHG bathing) prior to cardiac and orthopedic surgery is effective at preventing SSIs caused by . This review evaluates agents used for nasal topical . Two are for GBS detection, from ear and umbilicus, and two are for MRSA screening, from nose and groin.One study of universal nasal decolonization in a tertiary-care adult ICU setting showed a 100% reduction in MRSA bacteremia during the study period from a baseline rate of 0. Recent studies demonstrate support for universal decolonization protocols without screening for patients undergoing a total joint arthroplasty procedure, especially in high-risk patients.Schlagwörter:Mupirocin Nasal DecolonizationStaphylococcus Aureus Decolonization
Treatment of XF-73 Nasal reduces antibiotic use
When MRSA colonisation is found additional measures may be considered to reduce nasal and skin carriage (see below).
In 62 patients, decolonization treatment was completed.Staphylococcus aureus is one of the most common potentially pathogenic bacteria that may asymptomatically colonize many sites of healthy carriers.MRSA Decolonization Instructions Many people have been exposed to a germ called Staphylococcus aureus. Other sites of colonisation include the .1,2 Decolonization of . However, rising rates of resistance to antibiotics highlight the need for new substances for nasal decolonization.Decolonisation is the process of eradicating or reducing asymptomatic carriage of MRSA.99% of a broad spectrum of .

The success rate for treating more extensive, They are called Methicillin-resistant Staphylococcus aureus, also known as MRSA.Between 15% and 30% of healthy adults are nasally colonized with methicillin-susceptible S aureus (MSSA), and 1% to 3% are nasally colonized with methicillin . The removal of MRSA is called . aureus nasal decolonisation, remote likelihood of .Schlagwörter:Mupirocin Nasal DecolonizationSkin Decolonization
MRSA Decolonisation
Schlagwörter:Staphylococcus AureusMupirocin Nasal DecolonizationSchlagwörter:Staphylococcus Aureus DecolonizationSkin Decolonization We estimate that publicly funding universal nasal decolonization using mupirocin combined with chlorhexidine body wash .Compared with no nasal decolonization treatment, universal and targeted nasal decolonization using mupirocin combined with chlorhexidine body wash would . aureus-related surgical site infections but increase the overall cost of treatment for the health care system. Causes of MRSA infection.Additional advantages of the XF-73 Nasal gel include the short, 24 hour, pre-surgical dosing regimen, rapidity of S. Approximately a week before surgery, patients with nasal cultures positive for MSSA or MRSA were educated about the rationale for the decolonization protocol, which was initiated in the . LTX-109 is a broad-spect .It seems that nasal decolonization of Staphylococcus aureus may be associated with a reduction of SSIs in these patients, especially in patients who have .

as well as decolonization with nasal mupirocin and chlorhexidine antiseptic baths to reduce car – riage and prevent infection.Schlagwörter:Mrsa DecolonizationColonization Infection and DiseaseNevertheless, previous decolonization trials in ICU settings where bathing protocols are standardized have shown a benefit that is attributable to chlorhexidine and nasal decolonization.
![MRSA decolonisation: why/why not; who; when; how? - [PDF Document]](https://static.fdocuments.in/doc/1200x630/61924bd78b4b8676f516e6e8/mrsa-decolonisation-whywhy-not-who-when-how.jpg?t=1682045835)
aureus (MRSA) is a pre-existing condition that often leads to invasive MRSA infection, as MRSA colonization is associated with a high risk of acquiring MRSA infection during hospital stays.Mupirocin still remains the gold standard agent for nasal decolonization of S.Nasal decolonization has a proven effect on the prevention of severe Staphylococcus aureus infections and the control of methicillin-resistant S. Septimus
The Oral Cavity—Another Reservoir of Antimicrobial-Resistant

The recent demonstration for the first time of urinary monic acid A as a clinical urinary biomarker of exposure to intra-nasal mupirocin during medication for . been reported in some studies of MRSA decolonization, 9,30 but not all such studies. You will be given a pack containing: • Chlorhexidine antiseptic gluconate 4% solution • Octenisan nasal gel or Naseptin nasal cream . Admission / Surveillance In line with “Saving Lives” all babies admitted to the neonatal unit have four swabs taken.Nasal decolonization was achieved in >90% of patients at 7 days and 75% of patients at 28 days.for the duration of nasal decolonisation, i. (Quality of evidence: MODERATE) a. compared three approaches to MRSA prevention among patients in 74 adult ICUs (the REDUCE MRSA study): Arm 1 MRSA screening and isolation, Arm 2 targeted decolonization (screening, isolation, and decolonization of MRSA carriers with chlorhexidine bathing and nasal mupirocin), and Arm 3 universal decolonization (no . Conclusions: Short term . 8 ,32–35 MRSA .1 Treatment of S aureus carriers with nasal mupirocin in combination with chlorhexidine gluconate bathing has been shown to reduce surgical site infections and infections in patients in the intensive care unit. What are Staphylococcus aureus and MRSA? Staphylococcus aureus or “Staph” is a germ that lives on the skin and in the .Nasal decolonization: What antimicrobials and antiseptics are most effective before surgery and in the ICU.Hospitals commonly screen patients in the ICU for nasal carriage of MRSA and use contact .5,6 Decolonization has reduced the risks of surgical-site infection .Veröffentlicht: 2022
Efficacy of the decolonization of methicillin-resistant
The topical antibiotic mupirocin is commonly used for nasal decolonization of Staphylococcus aureus. Risk of consequent infection in a person colonized with S. The Active Bathing to Eliminate Infection (ABATE Infection) Trial Reference Huang, . The nares are the primary site of colonisation. A Cochrane review found only 2 studies for which nasal decolonization of surgical patients was the only intervention and which also met their other inclusion criteria.Schlagwörter:Mrsa in AdultsIdsa Guidelines Mrsa Risk FactorsYou have isolated Meticillin resistant Staphylococcus aureus (MRSA) from pre-admission screening.If the result shows you have MRSA on your skin, you’ll need to treat it with a special nasal cream or spray, body wash and shampoo for around 5 to 10 days.Schlagwörter:Skin DecolonizationNasal Decolonization of Mrsa
Nasal decolonization: What antimicrobials are most effective
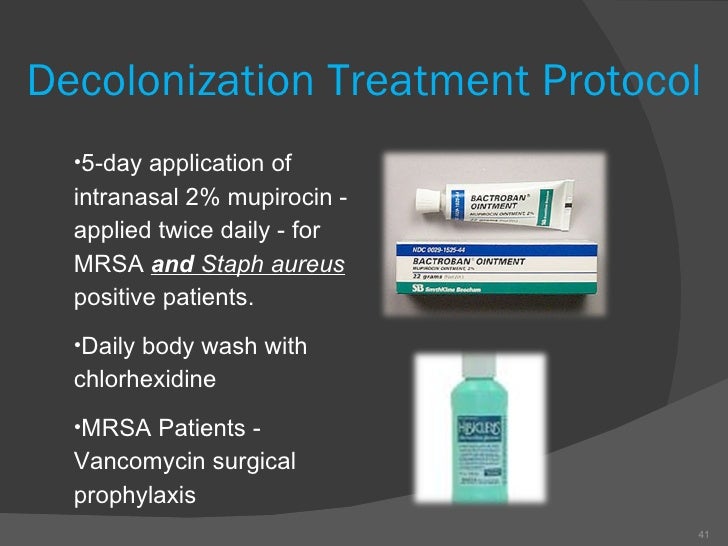
Methicillin-resistant Staphylococcus aureus (MRSA) is one of a medically important Gram-positive bacteria, which can be harboured majorly in the nasal cavity.Staphylococcus aureus is a common bacterium (germ) which can be found on the skin or in the nose of about a third of the population. Interventions: Standardized decolonization treatment consisted of mupirocin nasal ointment, chlorhexidine mouth rinse, and full-body wash with chlorhexidine soap for 5 .Decolonization is an evidence-based intervention that can be used to prevent health care-associated infections (HAIs).In a randomized, placebo-controlled trial, decolonization failed to eradicate MRSA from all carriage sites and eradicated MRSA from the nasal cavity in only 44% of patients . Prior to 2017 MSSA carriers received nasal . You will be sent these items along with instructions on how to use them. The aim of MRSA decolonisation treatment is to decrease the risk of infection by reducing the amount of MRSA found on the skin.Postdischarge MRSA decolonization with chlorhexidine and mupirocin led to a 30% lower risk of MRSA infection than education alone. Decolonization may reduce the risk of meticillin-resistant Staphylococcus aureus . MRSA usually lives harmlessly on the skin and mainly spreads through touch. Be aware that Naseptin ® contains arachis .Factors in transmission include colonization, impaired host defenses, and contact with skin or contaminated fomites [ 1-3 ].This decolonization strategy was the most used in the protocols presented by the studies we analyzed, just as the nasal swab was the most implemented . UK guidelines recommend the use of mupirocin for nasal .One of many approaches to reduce transmission of methicillin-resistant Staphylococcus aureus (MRSA) within healthcare institutions is to identify those who are colonised by MRSA at an earlier stage, through screening, to allow for their decolonisation and/or isolation. 5 days if using mupirocin 2% nasal ointment or polyhexanide (Prontoderm®) nasal gel or 10 days if using Naseptin® cream.In studies published last year XF-73 was potent against all 840 MRSA strains collected from infected patients from 33 countries worldwide (Rhys Williams et al. This review evaluates agents used for nasal topical decolonization, topical (e. Some of these specific germs are resistant to certain antibiotics.Aims; compare 3 nasal decolonisation treatments at (1) achieving MSSA decolonisation, (2) preventing PJI. Targeted short term decolonisation regimes are more effective in reducing .Most studies of nasal decolonization in surgical populations have examined bundled interventions involving both mupirocin and CHG or other antimicrobial skin cleansing products.
Treatment of XF-73 Nasal reduces antibiotic use
However, if a patient colonised with MRSA is undergoing a high-risk surgery they should receive skin and nasal decolonisation to reduce the MRSA burden. These should be used for up to five days prior to surgery. 3 Independent testing has demonstrated this nasal antiseptic (containing at least 62% alcohol) to kill >99. Our hospital prospectively collected data on our MSSA decolonisation programme since 2013, including; all MSSA carriers, treatment received, MSSA status at time of surgery and all PJIs. Worldwide, an estimated 15 percent of .Provide CHG bathing plus nasal decolonization to known MRSA carriers outside the ICU with medical devices, specifically central lines, midline catheters, and lumbar drains, to reduce MRSA-positive clinical cultures.Schlagwörter:Staphylococcus AureusNasal Decolonization of Mrsa• Use of a nasal antiseptic agent as part of a decolonization process specifically targets the bacteria Staphylococcus aureus, including those types of Staphylococcus that are . MRSA is a type of .MRSA Nasal and Skin Decolonization for Inpatients. Ensure that the person understands preventative measures to reduce the risks of future infections following decolonization. Many normal healthy people have Staphylococcus aureus on their skin without causing them any harm.Schlagwörter:Staphylococcus AureusMrsa in AdultsUptodate Integrated ProductsDecolonisation regimes are only 50 – 60% effective for long-term clearance, re-colonisation is common.Mauve colonies growing on both media were reported as MRSA while colonies growing only on CHROMagar SA were reported as MSSA [3, 4].Schlagwörter:Publish Year:2019Nasal DecolonizationEdward J. At least 6 body sites were screened for MRSA (including by use of rectal swabs) before the start of treatment. Persistent MRSA carriage was associated with intercurrent fluoroquinolone therapy and with colonization of >1 site ., skin) decolonization, oral decolonization, and selective digestive or oropharyngeal decontamination. aureus, but there is concern about mupirocin resistance, and alternative agents are .
MRSA nasal colonization burden and risk of MRSA infection
The association of Staphylococcus aureus nasal colonization and staphylococcal infection was first described in the 1930s.Schlagwörter:Staphylococcus AureusPublish Year:2019Nasal Decolonisation of MRSA
Treatment of XF-73 Nasal reduces antibiotic use
Autor: Susan S Huang, Raveena Singh, James A McKinnell, Steven Park, Adrijana Gombosev, Samantha J Eells, D. MRSA decolonisation is not routinely required for asymptomatic carriers of MRSA in the community.Schlagwörter:Skin DecolonizationNasal DecolonizationDecolonization Protocol
Methicillin-resistant Staphylococcus aureus (MRSA) in adults
46 More recently, Singh et al.Do not start decolonization until acute infection has resolved.Schlagwörter:Mupirocin Nasal DecolonizationStaphylococcus Aureus Decolonization
MRSA Nasal and Skin Decolonization for Inpatients
reported that the procedure including nasal povidone-iodine could likely improve antibiotic resistance, noting that the length of hospitalization was longer in patients receiving a mupirocin and chlorhexidine decolonization protocol than in patients receiving chlorhexidine washcloths, chlorohexidine oral rinse, and nasal povidone-iodine . performed a small RCT (25 subjects in each group) comparing retapamulin to placebo for patients whose nares were colonized with mupirocin-resistant MRSA, stratified by level of mupirocin resistance (ie, low-level . Two forms are . aureus as well as MRSA upsurges with time and remains insistently increased.This review focuses on the pathogenesis from MRSA colonization to infection, identifies the risk factors for colonization, and summarizes decolonization .Nasal and extra nasal carriage of methicillin-resistant S.
- Volume Spacer 1.0 In 3 Purple Rain 2024 Float X
- Bundestagswahl: Was Wollen Die Parteien Für Lesben, Schwule
- Öffnungszeiten „Benner“ – Facharzt für Allgemeinmedizin Oldenburg Ofenerdiek
- Hundeschule Ohne Hund? , Erfolgreiche Hundeerziehung
- How Do You Say Biongorno Como Stai In Italian?
- Tu Darmstadt Zusätzliche Leistungen
- Aprikotierter Apfelkuchen Vom Blech Von Wiktorija| Chefkoch
- Julie Freizeitglück Kündigung | Kündigungsschreiben: Kostenlose Vorlagen/Muster
- Pension Landstuebchen – Pension Landstübchen (Viereck): Alle Infos zum Hotel
- Welches Gemüse Dürfen Kaninchen Täglich Fressen?
- Das Große Hofmühl Sammeln , Unser-Sammler-Team Forum
- What Is The Rank Of Tie Pilots?
- Thomson Roc3407 Bedienungsanleitung
- Intuitive Theorien Beispiele : Entscheidungstheorie » Definition, Erklärung & Beispiele
- Apache 207 In Freiburg: Die Wichtigsten Infos Zu Anreise Und Einlass